The Vicious Cycle of PTSD and Sleep Disruptions
For many veterans, sleep issues and post-traumatic stress disorder (PTSD) go hand in hand. Research shows that sleep disturbances not only contribute to the development and severity of PTSD but also impact how well someone responds to treatment (Colvonen et al., 2019; van Liempt et al., 2013).
In other words, PTSD makes it harder to sleep, and poor sleep makes PTSD symptoms worse—creating a frustrating and exhausting cycle that modern medicine often fails to break.
Through my research and work with VETS, I’ve had the opportunity to see firsthand how ibogaine—a powerful psychedelic compound—has helped veterans with PTSD. One of the most encouraging outcomes? A significant improvement in sleep.
Why Sleep Is Essential for PTSD Recovery
Sleep is more than just rest—it plays a crucial role in emotional and physical health. During deep sleep, the brain processes emotions, consolidates memories, and regulates cognitive function. For individuals with PTSD, traumatic memories often remain unprocessed, leading to intrusive thoughts, flashbacks, and nightmares. Many also struggle with:
- Frequent awakenings or restless sleep
- Night sweats
- Sleep paralysis
- Increased anxiety and hyper-vigilance
Without quality sleep, emotional regulation becomes even more difficult. Irritability, mood swings, and heightened stress levels make it harder for veterans to function day-to-day. Breaking this cycle of sleep disruption is a key step in PTSD recovery—which is where ibogaine may play an important role.
Ibogaine and Sleep: A Missing Piece in PTSD Treatment
Psychedelic-assisted therapy has gained attention for its effectiveness in treating PTSD, depression, substance use disorders, and other mental health challenges. However, limited research has examined its impact on sleep—until recently.
A study conducted by Stanford Brain Stimulation Lab’s Brain Stimulation Lab found that ibogaine, a plant-derived alkaloid, significantly improved sleep in combat veterans (Faerman et al., 2023). This suggests that ibogaine’s therapeutic effects may extend beyond alleviating PTSD symptoms, offering a potential breakthrough in restoring healthy sleep patterns.
VETS’ internal data reinforces these findings. In post-treatment surveys, only 7% of grant recipients reported “good” or “very good” sleep before treatment. One year after receiving psychedelic therapy, that number increased to 77%. These results highlight ibogaine’s potential not just for addressing trauma, but for helping veterans regain one of the most fundamental components of healing—restorative sleep.
As the field of psychedelic-assisted therapy grows, continued research is crucial to further understand the mechanisms behind ibogaine’s impact on sleep and PTSD. Expanding clinical trials and gathering longitudinal data will help shape future treatment options for veterans in need.
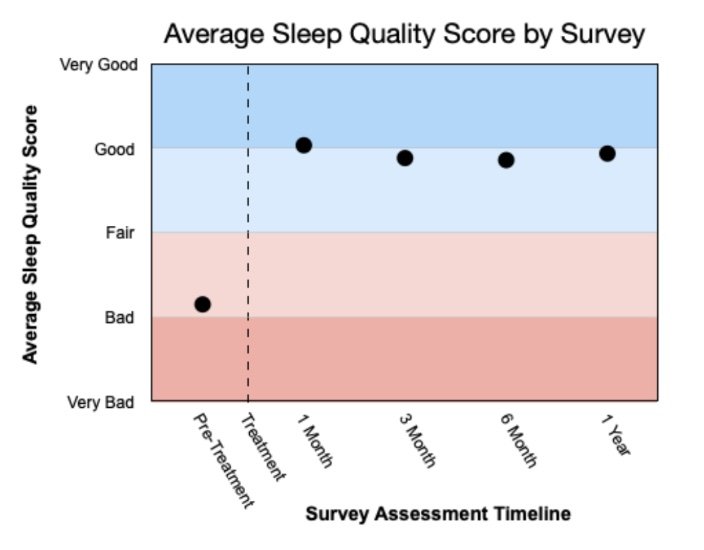
Source: unpublished internal survey data
The Future of Psychedelic Research for Sleep and PTSD
As psychedelic-assisted therapy continues to gain traction, more research is needed to fully understand how ibogaine impacts sleep and PTSD symptoms. Expanding clinical trials and long-term studies will be key to shaping future treatment options for veterans who need it most.
At VETS, we remain committed to supporting research and advocacy efforts that expand access to these transformative therapies. For those struggling with PTSD and sleep challenges, hope is on the horizon—and the science is catching up.
About Dr. Lori Camper, VETS Program Director
Dr. Lori Camper has worked with Special Operations Forces (SOF) families for over a decade, focusing on solutions for the unique stressors they face. She holds a PhD in Psychology with a specialization in trauma and crisis counseling and is a certified Psychedelic Integration Coach.
For her dissertation, she conducted a qualitative study exploring the lived experiences of SOF veterans undergoing psychedelic-assisted therapy with ibogaine and 5-MeO-DMT.